She had been alone in the electronic waiting room for a long time. Yet the face that appeared in the two-dimensional window was composed and thoughtful as she tilted her head to show the angle of her right jaw. ‘It’s my ear,’ she said. ‘It’s hurting something fierce.’ She brought the smartphone closer to her ear canal, so that its camera might show what lay within. But without lighting and an otoscope, all I could see from where I sat was a dark, blurry hole that filled the computer monitor.
Welcome to the hybrid clinic. In my case, it’s part of the East Baltimore Medical Center, about a mile from Johns Hopkins University Medical School where I teach, and even closer to the city jail and juvenile detention building. The waiting room is packed today. A row of exam rooms bear signal flags coloured red, yellow, blue, green. The signal flags let me know if a patient is waiting; if a patient has been seen; if a lab result is waiting; or if a patient is ready to go. Urgent-care doctors can easily fall behind schedule, so I’m used to keeping an eye on the hallways to see how many people are waiting for me. For those beaming in for a telemedical encounter – now roughly a quarter to a third of the patients on my schedule – it’s harder. There are no coloured flags in the hallway. While I had been scanning the clinic, she had been waiting a half-hour in the ether, and I hadn’t noticed. Telepresence is not the same thing as presence.
She accepted my apologies with an easy wave and moved on. ‘I don’t know what happened, but this ear pain just won’t go away,’ she said. ‘It’s like the time when I was cleaning out my ear with a bobby pin and my daughter jumped out and surprised me and I pushed the bobby pin all the way into my ear.’ She paused. ‘Except this time there was no bobby pin.’ Was any bloody discharge coming from her ear? No. Was there fever or chills, nausea or vomiting? No. Was her hearing affected at all? No. Was there anything meaningful I could do through this link connecting my clinic to her smartphone? No.
The physician Clarence John Blake would have sympathised. In 1880, this founding faculty member of the Massachusetts Eye and Ear Infirmary struggled with the limits of medical care by telephone. He recalled with some humour how quickly he and his colleagues had conjured new, far-reaching applications for the new phone, immediately after the first demonstration by Alexander Graham Bell in 1876. They envisioned a new specialty of telephone consultants who ‘would each settle themselves down in the centre of a web of wires’ and listen to ‘the heart-beats of a nation’, diagnosing and treating patients at a distance. But four years later the promise had not come to pass. Of the many new gadgets proposed to help make telephones into long-distance stethoscopes, Blake sighed, ‘none have as yet, even in a slight degree, answered this purpose.’
Blake had been one of the first to see the medical potential of the telephone. His predictions spread along with sensational stories of ‘tele’-medicine, like the 1879 report of a teledoctor in Cincinnati that appeared both in the Journal of the American Medical Association and in The British Medical Journal. Late one night, a physician in Ohio was summoned by a caller who feared his coughing child had a bad case of the croup: a true emergency. Instead of making a midnight ride to the house of the caller, the technologically savvy physician asked the father to simply ‘hold his child for a few moments before his telephone’. Using the phone as a long-distance stethoscope, the ‘practised ear of the physician’ determined the cough was not croup; there was no emergency. Father, child and physician were all able to go back to sleep, and by the time the physician saw the patient in the morning ‘all symptoms of laryngismus stridulus had disappeared, and the child was apparently quite well.’ The fortuitous story of the careful and clever Cincinnati paediatrician and his fortunate little patient was not how most telemedicine encounters went, however.
In his audiological research and clinical practice, Blake simply could not translate the theoretical abilities of the telephone into the practical demands of everyday care. His attempts to use the telephone as a stethoscope reported no positive results, except ‘in one instance only, of the suspicion of a barely perceptible “thud”, no sound which could be referred to the heart as its source was heard.’ Instead, he heard all sorts of artefacts. These ambient and distorted sounds came from the electrical grounding of the device: ‘the snapping and crackling noises indicative of earth currents, the clicking of the Morse instruments, and the sound of a “fast speed transmitter” on the Western Union lines running along the Providence railroad, and the ticking of the clock connected with the Observatory in Cambridge.’ The ‘web of wires’, as Blake put it, failed to create a specialty of telephone medicine, in part because of ‘the very delicacy of the telephone … and its almost fatal propensity – if such an expression may be used – to pick up sounds that did not belong to it.’ Sometimes, the telephone brought too little information, sometimes it brought too much.
The promise of telemedicine may be much closer at hand now than it was a century or so ago
The web of wires that extended into hospital, clinic and home brought about new understandings of an electronic network as both an abstract concept and a material thing. In the early 20th century, hospitals modernised and grew more and more specialised, and telephone wires formed its rapidly branching nervous system. As telephones became a common feature of the middle-class home, and patients increasingly used them to call their doctors, a new form of telephone triage soon became part of medical practice. When was it OK to give medical advice over the phone? And when was it dangerous to do so? What kind of ailments, like the ear complaint I was being called to see, required the presence of the doctor or the body of the patient? When was telepresence ‘good enough’ for medical practice – and when was it just a form of substandard care?
There are vast differences in the social norms of technology and the political economy of care that separate the medical use of the 19th-century telephone from the health apps of the 21st-century smartphone. As a physician, however, in my hybrid clinic every week of the ongoing COVID-19 pandemic, I have found some similarities too. Some limitations of practising medicine through electronic media link the frustrated 19th-century ear doctor and the frustrated 21st-century ear patient. They are not solvable by better tech. The promise of telemedicine may be much closer at hand now than it was a century or so ago – as close as the smartphones found in the pockets or purses of more than 85 per cent of the US population. Yet the fact remains that some forms of care require more physical presence than others.
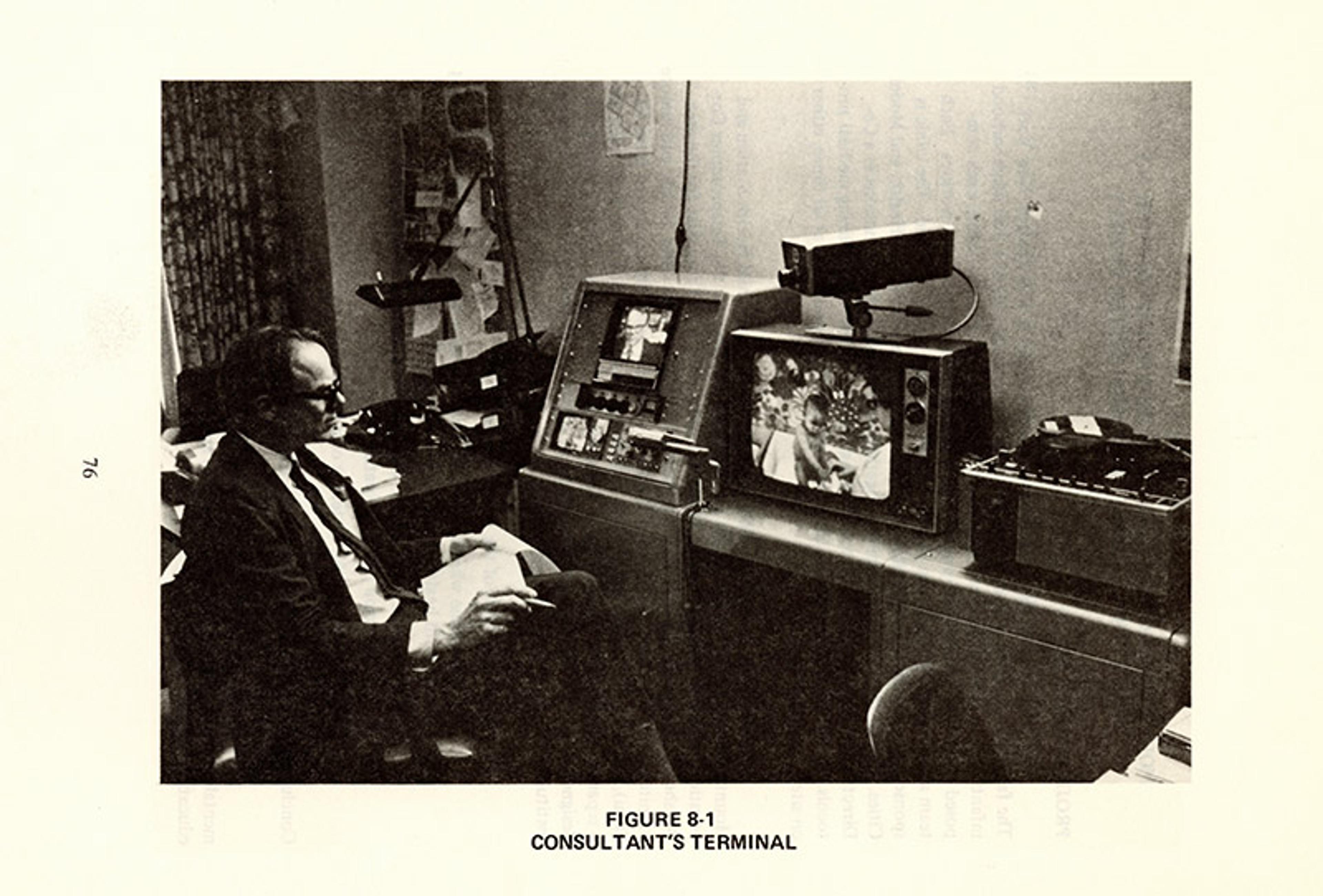
The platform we now call telemedicine or telehealth was born of frustration with the limits of the technology of the telephone. Kenneth Bird, the Boston-based physician who coined the term ‘telemedicine’ a half-century ago, thought that television could solve the shortcomings of telephone medicine. At the time, Bird staffed his own hybrid urgent-care clinic at Boston Logan International Airport. The doctor was in person during peak commuting hours, and on call by telephone and pager for the nurses who staffed the clinic 24 hours a day. One of his first telephone patients had a hip injury too tricky to understand over the phone, and had to be sent to the hospital. ‘If only I could see the patient,’ Bird thought, he could have saved her that ambulance ride. ‘If I could see a space launch 1,000 miles away in Florida, and hear an astronaut’s heartbeat 1,000 miles up in space,’ he continued, ‘then there was no reason why a patient a few miles away couldn’t be seen and his vital signs checked, while a nurse led him through a physical examination.’
A grant from the US Public Health Service, a collaboration with local TV engineers, a set of specialised cameras, microwave towers and a lot of coaxial cable allowed Bird to transform the tiny airport clinic into a ‘wired clinic’. Its cameras patched directly to a special multimedia room in the Massachusetts General Hospital.
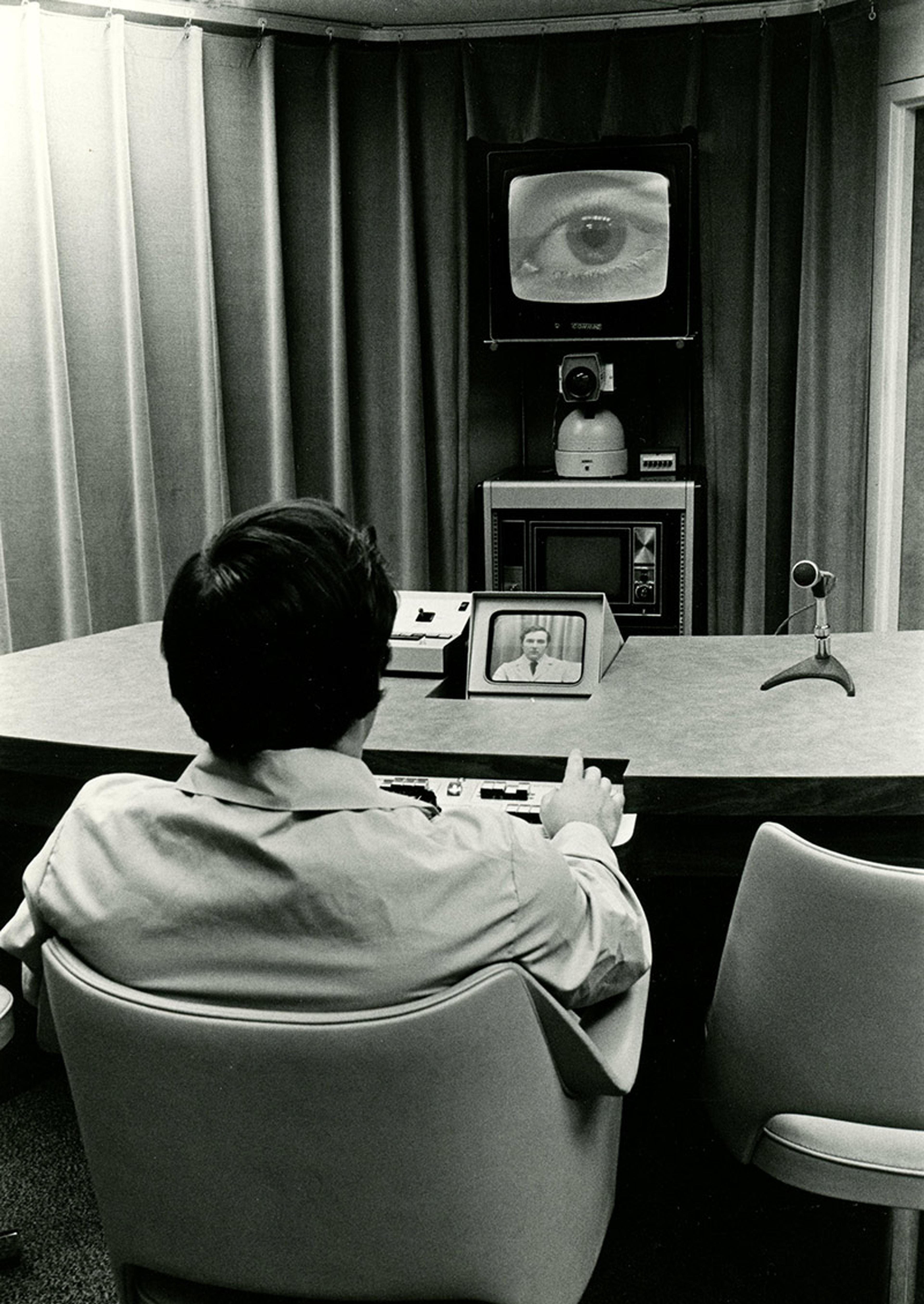
Telepresence, to Bird, permitted a ‘dynamic interaction which allows interpersonal communication across distance to recreate, and even enhance [my emphasis], face-to-face communication.’ Bird drew heavily on the media theorist Marshall McLuhan, especially his observations that, in the electronically interconnected society of postwar America, ‘ours is a brand-new world of allatonceness’, as he and his co-author Quentin Fiore put it in The Medium Is the Massage (1967): ‘“Time” has ceased, “space” has vanished.’ So too with the clinic: the teledoctor defined ‘telemedicine’ as ‘the practice of medicine without the usual physician-patient physical confrontation’. Interactive television created new possibilities of being together, even when apart.
He hoped the TV frame could engineer more than ‘good enough’ medicine; it could deliver better medicine
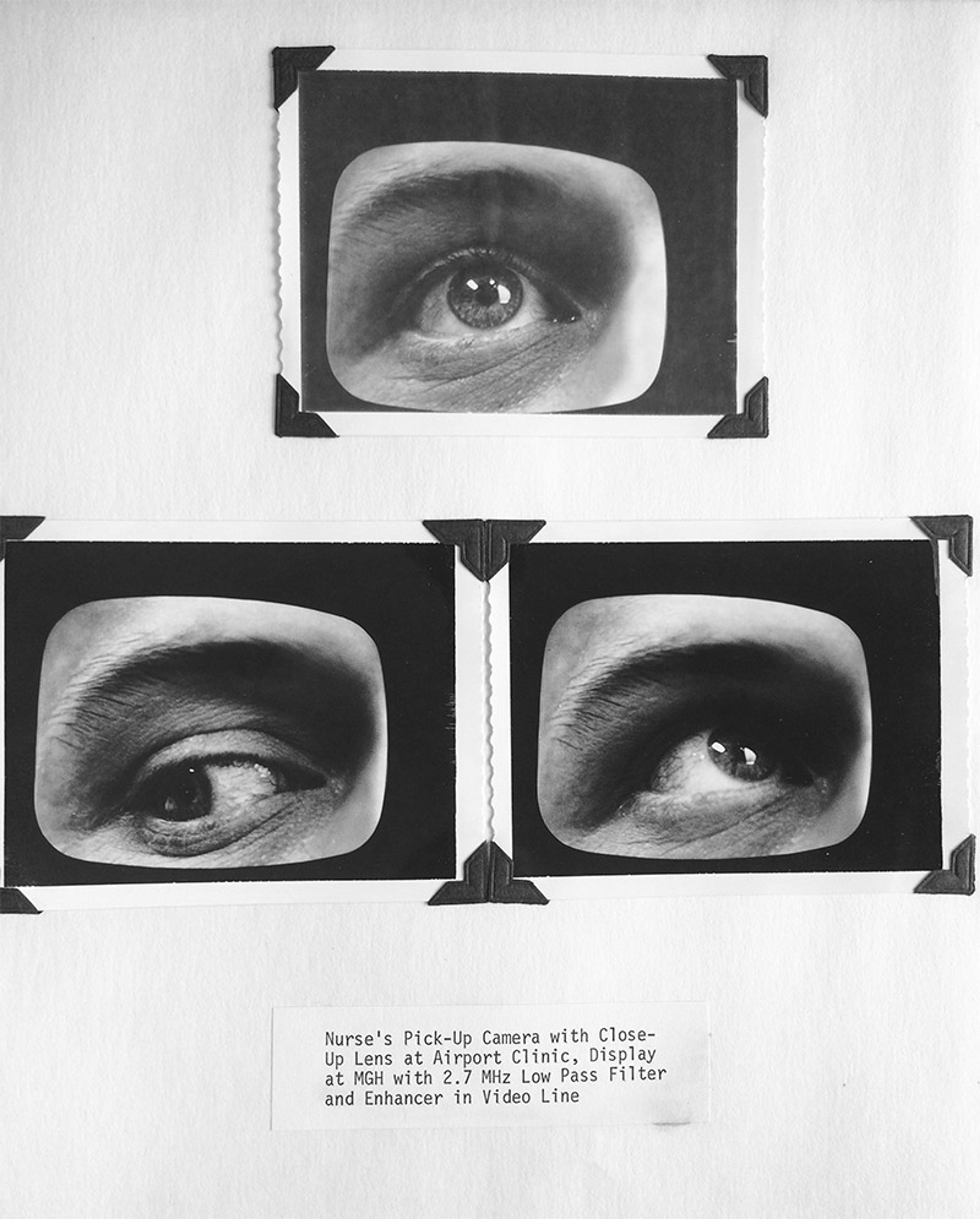
Telepresence brought peril as well as promise. How could a doctor or patient know whether the video quality was good enough to simulate the face-to-face presence of a direct physical examination? Artefacts or poor focus might lead to a missed diagnosis. Measures of parity obsessed Bird and the TV engineers who set up the clinic. They assembled archives of visual data to establish where, exactly, to set the threshold of ‘good enough’ diagnostic image quality. If a doctor could see a lesion in the blood vessels of the conjunctivae in person – that is, the red streaks in the ‘whites’ of your eyes – would that same lesion be visible to another doctor looking at that eye on a TV screen several miles away? Consider the photographic prints pasted onto the page in the figure below, depicting three television screens, which themselves depict images of the eye exams of a model patient at three different camera settings. In hundreds of images like these, testing the influence of different permutations of cameras, lenses and video-enhancement algorithms on the ability to distinguish key features on microscopic, radiological and physical examinations, Bird launched a new science of similarity, documenting the equivalence of telepresence and physical presence.
In a well-designed telemedical interface, argued Bird in a 1970 paper co-authored with the lead nurse practitioner Marie Kerrigan, ‘the fundamental doctor-patient relationship is not only preserved, but often it is actually augmented, enhanced, and seemingly more critically focused.’ Let’s consider the terms more closely, as Bird and Kerrigan did. Bird’s microwave transmitters ‘augmented’ the signal to travel long distances; he developed image ‘enhanced’ filters for TV signal processing; and the ability to shift between wide-angle and long-lens cameras allowed his teleclinic to be ‘critically focused’. In his more expansive moments, Bird hoped the TV frame could engineer more than ‘good enough’ medicine; it could deliver better medicine. ‘Telemedicine can provide as much or more [my emphasis],’ he insisted, ‘than the actual physical presence and direct interviewing of the physician.’ Despite these hopes, in fact many doctors and patients found telepresence to be a poor substitute for physical presence.
Television medicine provided more modes of contact than telephone medicine, but was still limited to sight and sound and the constraints of the camera frame. The absence of touch, of smell and of the sensibility we use to navigate interpersonal interactions persisted. The sociologist Joel Reich, in a 1974 report on telemedicine that took Bird’s clinic as its principal model, tried to catalogue all the things not present in telemedical encounters. Reich’s account of telemedicine is a history of the senses: visual and aural were present, yes, but olfactory, gustatory, thermal and haptic channels were not. They were all missing, and their absence was crucial.
‘Until such a time as Smell-o-Vision became a reality,’ Reich half-joked, ‘with contemporary interactive television the loss of the olfactory channel is complete.’ Reich compiled a list of roughly 50 diseases for which the use of smell might still play a part in routine diagnosis. The clinical significance of losing smell (and taste, for that matter) was minuscule, but they were losses all the same. Nor was it clear that a nurse practitioner, standing in the same room as the patient, could develop an adequate language for describing odours verbally to a physician on the other end of a telemedical circuit. A similar concern related to the relevance of colour. Bird’s studies of visual thresholds for telemedical parity assumed black-and-white television was more practical for telediagnosis. When colour was relevant, for example, when diagnosing a skin rash, practitioners on both ends could refer to numbered codebooks (analogous to the Pantone Color chart) to convey the right colour. Colour could be standardised and rendered legible at both ends of the black-and-white television circuit in ways that smell could not.
These losses paled in comparison with losing touch, or the ‘haptic channel’. Some elements of touch, like the sensation of hot and cold, could be captured using thermometric sensors and transmitted electronically as graphs, charts or raw numerical data. Yet the single quantum of temperature could not contain all the qualitative information captured by a physician’s hand on a clammy brow. The haptic channel also works two-ways: the hand of the physician is both a sense organ and a means of providing communication, reassurance, a form of therapy in its own right. Another hand, perhaps that of a nurse practitioner in the same room with the patient and the television camera, might act as a limited prosthesis for some of these functions, but not all.
The problem of presence and absence is coupled to the matter of justice and fairness
Bird suggested that other technologically mediated senses and agreed-upon codes of interaction would compensate for the loss of touch. ‘There are several uses of telemedicine circuitry,’ he noted, ‘in which a modification of the normal co-presence ritual may have to be considered eventually.’ After all, wasn’t our own presence in the three-dimensional world in part a construct of our shared social reality, a set of etiquettes and protocols that had evolved over millennia but could be re-engineered to work, perhaps better, in electronic forms? Just as deep-sea divers learned to communicate with coded hand gestures in a benthic environment that did not permit oral communication, doctors and patients could figure out new codes for telemedicine.
Bird focused on proofs of parity, and since then much of the scientific literature on telemedicine has likewise been concerned with demonstrating that the services provided by medicine at a distance are equivalent, even if not identical, to those provided by flesh-and-blood encounters. This evidence is uneven: well-developed in the highly visualised fields of radiology and pathology, or in tele-vanguard fields of psychiatry, neurology and cardiology. It is harder to document in more generalist fields, including primary care internal medicine, obstetrics and gynaecology, and paediatrics, and especially difficult in procedure-based surgical fields. The difference between these fields is not absolute but relative. It is a difference of stakes and proof, and who faces the risks and costs if something is lost along the way.
Something is always lacking in telepresence, but advocates hope that this something is relatively trivial to the task at hand. If it is not, then the primary value of telemedicine (in offering access to care where care is otherwise absent) becomes a cynical falsehood. In truth, the problem of presence and absence is coupled to the matter of justice and fairness. If the difference between telepresence and presence is trivial, then insisting on presence in effect denies care to many who may not be able to visit in person. On the other hand, if the difference between presence and telepresence is significant, then the promotion of telemedicine becomes the endorsement of a debased form of ‘good enough, but not really good’ care. And if that second-class form of care is delegated to those who are already the victims of classism or racism or both, then telemedicine is constructing another form of segregated care.
Several times in the past century, an emerging communications technology has promised a means to knit together the divided fabric of US society, to integrate marginalised communities without needing to engage with the structural matters responsible for those divisions. In the 1970s, cable television promised to knit US society back together as a newly ‘wired nation’. ‘The stage is being set for a communications revolution,’ wrote the journalist Ralph Lee Smith, as ‘every home and office will contain a communications centre of a breadth and flexibility to influence every aspect of private and community life.’ Just a few years earlier, the report of the US president Lyndon Johnson’s National Advisory Commission on Civil Disorders (the Kerner Commission) had exposed in granular detail systemic inequalities in education, policing, employment, housing and welfare within US cities, and called for large-scale federal spending to redress them. Instead of following any of these recommendations, however, the Johnson administration commissioned a new Task Force on Communications Policy to evaluate the role that interactive satellite and cable television might play in healing the urban crisis in the US. ‘If it is true,’ Smith concluded in his book The Wired Nation (1972), ‘as it seems to be, that cable TV is about to effect a revolution in communications, it must be said that a revolution has rarely been created by persons of less revolutionary intent.’
In retrospect, it seems deeply misinformed to suggest that an information technology on its own could reverse the accelerating vector of postwar urban segregation. This process, whose origins can be traced serially through racially restrictive covenants, federal redlining maps, and brutal policies of urban renewal, systematically circumscribed and denied services to the predominantly Black and Latino communities they pathologised. Yet the promise of cable telemedicine had the ear of the federal Department of Health, Education, and Welfare and of the Rockefeller Foundation. These funders supported the emergence of a national telemedical network that would extend the benefits of modern medicine to marginalised and underserved populations. Cable TV could immediately connect physicians concentrated in affluent urban and suburban centres to underserved communities of the inner city and rural areas alike.
In the 1970s, the federal government sponsored at least 14 telemedical demonstration programmes. They were each designed to showcase the use of interactive television to counteract a different social disparity in healthcare access. These programmes targeted a variety of underserved populations, from rural white settlements in remote areas of Vermont and New Hampshire, to inner-city Latino and Black communities in Harlem and the West Side of Chicago. Other projects explored the potential of telemedicine in reducing the steep healthcare disparities found across Inuit and American Indian reservations from Alaska to Arizona, the rapidly industrialising island population of Puerto Rico, and the growing prison population of the Miami-Dade County Correctional System. The goal was to provide evidence of feasibility, efficacy and acceptability: to lay the groundwork for nationwide telemedical networks.
By 1972, the Wagner Homes clinic served 1,300 children, but lacked the budget to support a full-time physician
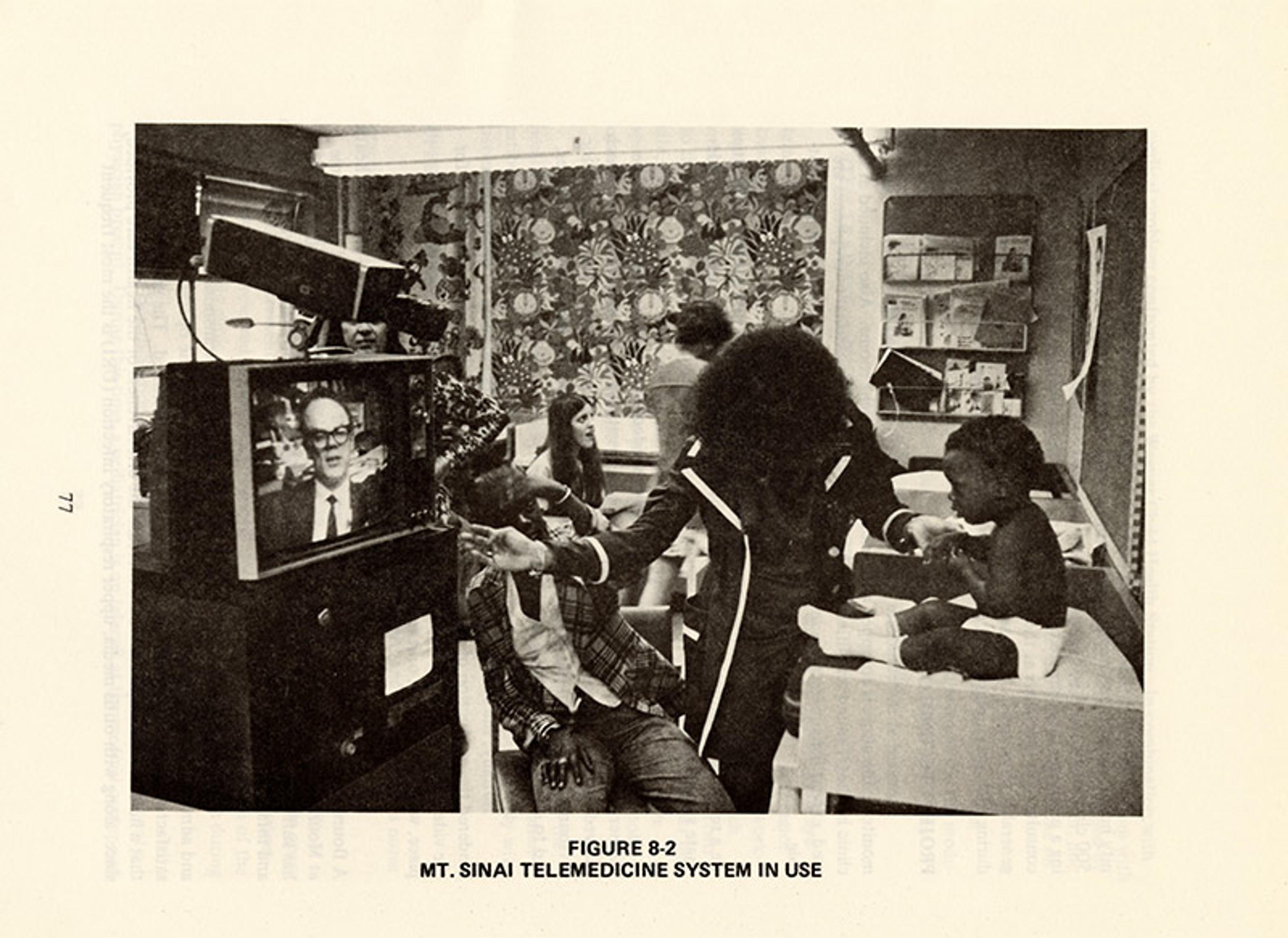
Harlem became an important site for imagining technological fixes to resolve what some called the ‘medical ghetto’. At nearby Mount Sinai Hospital, the Harlem native and second-generation physician Carter L Marshall proposed a telemedical solution to disparities in access to care. Marshall’s earlier work had emphasised the interplay of biological and social forces that shaped community health. He was aware that many East Harlem residents resisted setting foot in the hospital until they were so ill as to be beyond the reach of medical help. He hoped that the right kind of communications platform could help bring these people into care at an earlier stage of illness – and at an earlier stage of life. Marshall envisioned a paediatric outreach programme that would stretch directly from the Mount Sinai Hospital into the structure of Harlem’s tenements and public housing projects themselves, using medical television.
‘There are two ways you can look at problems that involve the delivery of health services,’ Marshall told The New York Times in 1973, shortly after establishing a telemedical link between Mount Sinai and a community health centre in the Wagner Homes Projects at 121st Street and Fifth Avenue. One of them is to fix the structure of the healthcare system itself. The other is to use technology to circumvent these fundamental problems. ‘Our interest here,’ he continued, ‘is how we can adapt technology to the delivery of health services, regardless of the organisational framework.’ Pointing to the Kerner Commission report on civil disorder and the subsequent focus on cable communications, Marshall suggested that Harlem was an ideal place to study the potential for cable television (CATV) to reduce disparities in access to healthcare. ‘We at Mt Sinai,’ he stated, ‘are in a unique position vis-à-vis CATV in that we are located in the franchise area of the TelePrompTer Corporation,’ and so could form a ‘unique partnership between a voluntary medical setting and the private sector of CATV.’
The timing could not have been better. New York’s mayor John Lindsay had just declared the city a model for exploring the social benefits of cable connectivity. TelePrompTer had just announced a new Harlem storefront studio on 125th Street. The company could point to recent programming on sickle cell disease as evidence of its commitment to use cable television to advance the health of the Black community. Reverend C T Vivian, head of the Harlem-based Black Center for Strategy and Community Development, called TelePrompTer’s move ‘the first time to my knowledge that an independent Black group has been able to develop a relationship with a CATV company that would allow for creative programming out of the Black condition on an independent basis.’ When TelePrompTer came under fire for not being a Black-owned business, it noted that more than half its workforce was made up of African American and Puerto Rican New Yorkers.
Federal funding for telemedicine was about demonstration, not implementation
TelePrompTer’s dedicated coaxial lines linked Mount Sinai’s high-tech hospital with a community clinic in the Wagner Homes projects. By 1972, the Wagner Homes clinic served 1,300 children, but lacked the budget to support a full-time physician. With continuous cable links, Marshall hoped full-time medical services could become available to more residents of Wagner Homes and surrounding public-assistance housing projects, encouraging Harlem residents to seek out formal healthcare. Each station had a TeleMation camera with a 9-inch direct video monitor and a 19-inch receiver, with wide-angle and zoom lenses and microphones. The clinic was staffed by nurse practitioners (who spent most of their time at the Wagner Homes clinic) and paediatricians (who spent most of their time at the Mount Sinai Hospital). In an early report to the National Cable Television Association, the Mount Sinai team explained their plans to expand the cable link to other health stations, schools, daycare centres and – ultimately – into every home in Harlem.
Yet many Black and Latino parents in East Harlem were wary of Mount Sinai. Well before the racism of the Tuskegee Syphilis Study by the US Public Health Service was exposed in 1972, activists in the Black Panther Party and the Young Lords Organization had criticised mainstream, private academic medical centres like Mount Sinai as indifferent at best and ‘genocidal’ at worst toward the minoritised communities who lived alongside their campuses. Many Harlem residents understood that recent shifts in federal and state healthcare funding – including the New York State Ghetto Medicine Program that funded private hospital outreaches to community health centres such as Wagner Homes – also threatened funding for public institutions such as the municipal Harlem Hospital. Mount Sinai was singled out by the chair of East Harlem Health Council, Robert Palese, as a private entity receiving ‘huge sums’ under the Ghetto Medicine Program, ‘without answering the health needs of the poor people in the community’.
The opening of the TelePrompTer storefront on 125th Street and the Mount Sinai demonstration in Wagner Homes both received extensive publicity. It was a success story that showed how cable television could bridge the ‘sociocultural gulf that separates inner-city residents from healthcare resources’. Yet the success of this federal pilot programme was followed by market failure. Having proved the efficacy of telecommunications with nurse practitioners, in 1975 the federally funded contract was terminated. As a spokesperson for the National Center for Health Services Research drily noted, the demonstration was successful at its stated goals and now ‘the project has gone about as far as it could go.’ Federal funding for telemedicine was about demonstration, not implementation.
The physician and civil rights activist John Holloman, who practised at nearby Harlem Hospital – warned that demonstration projects involving minority health were often more concerned with short-term gains than long-term commitments. ‘When a demonstration model designed and operated by whites proves to be unsuitable, no one makes a fuss about the inefficiency or inexperience,’ Holloman pointed out. ‘Someone simply writes it up as a part of the study, presents it at a conference, and then a new model is designed and tried until the best way is found to make things work properly. We [the Black community] must have the equal right to make mistakes, to fail, and to try again.’ Yet in these evaluations of communications technologies in community health, the purse strings were rarely held by those in the community. As a result, even when a programme like the Wagner Homes telemedicine project succeeded, the political and economic commitment to support it could still fail, all the same.
Wary as he was of demonstration projects, Holloman nonetheless held out hope that this demonstration might yet produce meaningful responses to enduring social problems. He continued to advocate for telemedical technologies as a bridge to equalise access to medical care. His position was just as pragmatic as any 21st-century actor trying to advocate for health equity using the eHealth, mHealth and wearable technologies of the present moment. As a new vehicle for bridging social divides, telemedicine – then as now – offers possibilities for improving public health and empowering communities. Holloman understood racism as a part of daily life – yet, if the long-term solutions to its problems required larger budgets and timescales, why not begin with smaller projects that could be operationalised on a shorter timescale, through laying a few miles of coaxial cable and hooking a camera to a television set?
That TV failed to resolve healthcare disparities might, in retrospect, seem inevitable. But understanding how the promise of a technological fix to a political problem can continue to hold enduring appeal for many who should know better just grows more urgent now.
Telemedicine has offered only a thin slice of health equity to the patients I serve, but that doesn’t mean it hasn’t provided anything. Nor did it completely fail the woman whose ear pain I was unable to diagnose via smartphone. I saw her again, towards the end of my shift, this time in an examination room off the main hallway. She was able to walk the few blocks over from her home in a nearby public housing project. There was some unpleasant weather along the way; her coat, hanging on a hook on the door, was still shedding its last few drops of water on the floor. But her ear was there too, and much easier to see. The outside of her ear was tender to touch. Her ear canal had an angry red line flecked with white discharge, but the eardrum looked healthy and pink.
An outer ear infection, then. Easy to treat with the right antibiotic drops, but hard to see on a smartphone. Could you design an otoscope attachment to snap onto the camera on her phone? Sure. Amazon, at latest check, had a few dozen of them for sale, some with built-in ‘earwax removers’ and ‘infection detectors’. Perhaps one day there will be a run on them as there was a run on pulse oximeters in the early days of the COVID-19 pandemic. But most patients I see don’t have blood pressure cuffs at home, they don’t have pulse oximeters at home, and they don’t tend to have digital stethoscopes or otoscopes either. In the hybrid clinic, the smart suite is not laid out evenly for all comers.
Like a grain of sand in the shell of an oyster, it might help to build something luminous and beautiful
My patient’s experience should not be taken as an example of the inevitable failure of telemedicine. Telemedicine still served her as a form of triage, and helped her find her way in to the clinic and ultimately to a successful cure. We need to understand that information technologies are always only a form of triage, a temporary patch that points towards the work to build a better medical system. Early telemedical technologies did not end health disparities, but for a little while they did enable federal funders and a coalition of stakeholders to come together around a shared goal of engineering equal access to healthcare. That is an example of how technologies can produce limited forms of social change, even if they cannot serve as replacements for long-term investment and political will.
The segregation of our medical system is not the same as it was when Holloman insisted that we turn our gaze towards, and not away from, our medical ghettos – but steep disparities and systemic racism continue to impact the experience and outcomes of healthcare in the United States. Although new technologies such as the telephone and the television could not themselves undo the political and social forces that drove systemic racism, argued Holloman in 1969, ‘telephonic and two-way closed-circuit TV can be established to link the ghetto physician to the medical centre, services that could be put into operation almost at once.’ These technologies were readily at hand. Why not use them?
It was not naive for Holloman to hope, a half-century ago, that a new tool might break the cycles of disappointment of the past. That the right technology could serve as a catalyst to level the steep asymmetries of access that characterised US healthcare. That it might be a nidus of change, like a grain of sand in the shell of an oyster, to help build something luminous and beautiful. Nor is it naive for us to want to believe, even today, that the new communications technologies through which medicine is now being practised might bend the arc of our bloated, inefficient and unjust healthcare system just a bit closer to that of the equitable and just society in which we hope to live.
But what Holloman saw so clearly then, we must now strive to remember: technology alone will never accomplish this uniquely human endeavour. The responsibility is ours to see it through.






