My patient was dead before I even saw her. She had been in a car accident. Now she was scheduled for organ donation.
She was called an ‘ASA 6’. To estimate operative risk, the American Society of Anesthesiologists (ASA) has a classification system built around how sick a patient is, ranging from a healthy ASA 1 to a moribund ASA 5, the latter meaning someone is not expected to live 24 hours. When the system was created in the mid-20th century, a sixth class for dead people seemed pointless. Death was known to the dead only, and life to the living only, and between the two there had been no bridge. When the definition of death changed in the late 1960s, making it possible for a person to be ‘brain dead’ but with organs still very much alive and available for donation, a bridge appeared and a sixth class was created in the early 1980s. Since 1988, when officials started collecting organ transplant data, almost a million organ transplants have been performed in the United States. Most of the organs have come from brain-dead donors. In 2021 alone, the US had almost 10,000 such donors.
When told of my upcoming case, I had mixed feelings. On the one hand, being in perfect health, unaccustomed to suffering and therefore easily disconcerted by the thought of death, I was horrified. My attitude toward death was like that of a young person standing blindfolded and tied to a post, awaiting a volley from a firing squad. The whole concept made my blood run cold. Yet the case also aroused in me a feeling of relief. Simply put, there was no risk of malpractice, as my patient was already dead. Many anaesthesiologists have such self-centred thoughts when taking care of ASA 6 patients.
In her early 30s, she had a youthful face, without the traces of severe illness that ICU patients typically have. With her hair wrapped inside a bright, polka-dotted kerchief, she gave off an expression of almost pleasant, good-humoured cheeriness.
Who was this young person whose life had been tragically snuffed out? I jabbed into every crack of her medical record to find out. But little had been written down. Both her life and death seemed simple enough to be chronicled in a few lines. Something had happened inside her brain with the car accident, and the end came.
We wheeled her toward the operating room. Before departing, I pulled the sheet over her exposed feet. Why? I had an objection to her being dead, but I had an even more serious objection to her being undignified. With my patient still partly in the world of the living, I wanted to keep a place for her in the part that pretends to be genteel.
Six hours she had been officially dead. Now she had re-entered the world of the living
When we arrived in the operating room, something turned over inside me, sank, and went cold. After all, she was dead. The day before, she was as whole as me – and now look. She would never rise again.
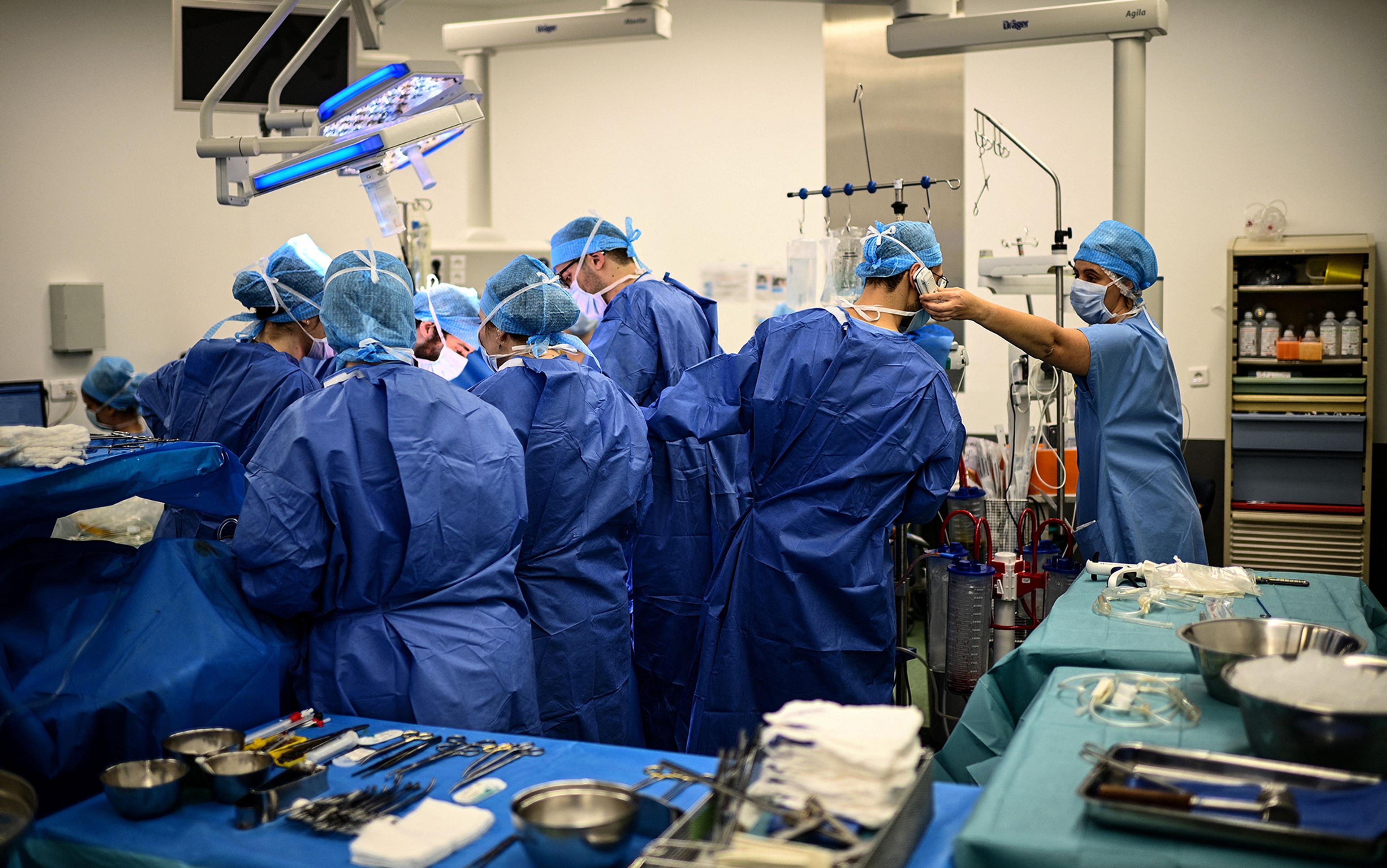
After we moved her from the gurney to the operating table, the doctors and nurses, so used to taking care of living patients, stared at one another stupidly, as if not knowing why they had come together or why they stood around the table. For a brief moment, each one of us likely had the same supernatural vision, how for the past six hours, after being declared brain dead, this woman had lain under the measureless power of death. Six hours she had been officially dead. Six times had the hour hand on the clock moved – and she had lain dead. Now she had re-entered the world of the living. I would support her blood pressure and pulse. I would make her blood bright red with oxygen. Indeed, she might even wake up and look at us, I fantasised. She might be raised from the dead.

In a race against time, Thomas Charrier checks a monitor during the operation to remove the donor’s lungs
Ghoulish thinking, yet I do not write about this case to be ghoulish. Nor am I trying to stake out a new position in the bioethics debate. My purpose is more practical. Today, artificial intelligence (AI) looms over medical practice. Although unlikely to replace doctors completely, AI makes some medical activities especially ripe targets for takeover, including the harvesting of organs from brain-dead donors. And why not? Bedside manner and the common touch cease to be concerns. Using AI machines rather than doctors to harvest organs also promises to save money.
Yet this impersonal, nonhuman method of organ retrieval may discourage people from becoming organ donors, or from letting dead relatives become so, thereby exacerbating the current organ shortage. People will see pictures of organ retrieval being carried on all around by inanimate machinery in a room completely abandoned by human beings. Bodies will be brought in and sent out, while the invisible, sleepless work of the machines goes on. ‘Please, tell me this is not my end,’ people will fret privately. And they will resist consenting to organ donation.
Organ retrieval can take place at odd hours because the time between retrieval and transplantation must be minimised. A donor heart or lungs can last only four to six hours outside the body. A kidney, liver or pancreas can last a bit longer. Because donation and transplantation must be synched perfectly, surgical teams must be allowed to work at any hour of the day.
Although donors are dead, managing their anaesthesia can be tricky. To keep their organs healthy, their physiology must be carefully attended to, yet brain death affects each organ system differently. High intracranial pressure can lead to an enormous outpouring of adrenaline, which can injure the heart and other organs as circulation fails. Brain death can cause pulmonary oedema (fluid in the lungs), making it hard to oxygenate the blood, thereby damaging the organs by a second route. Brain death also wreaks havoc on the body’s endocrine system, causing vital hormone levels to fall and damaging organs by a third route.
My patient lay stretched out on the table. The room was silent, as I had not yet placed any vital sign monitors on her body. It was a sinister silence. The monitors typically emit sounds that resemble the unconcerned twitter of birds. In an operating room, they symbolise life. Their absence suggests that a patient is not alive. In fact, mine wasn’t.
Nature will never permit anyone to know the exact point where brain death becomes real death
Ready to cut, the surgeon spoke through his headphones to surgeons in other cities waiting for the organs. The rest of us said nothing as he gave them an estimated time of arrival. The team had a real need for a stout word in these last few moments before the operation began. Sensing the mood, the surgeon said some dignified things about how our patient was giving other people a chance to live. Everyone nodded in agreement. He seemed thankful and sincere, yet he had to be that way for, at such a moment, anyone with even a modicum of intelligence would have felt anything else as an affront.

Removal of the donor’s lungs
The surgeon cut into the patient’s chest. Almost immediately the patient’s heart rate and blood pressure jumped. It resembled the powerful surge of life that comes during a period when a person’s very existence and survival are at stake. The jump originated in a spinal reflex that stimulated the woman’s sympathetic nervous system below the level of the brain. Still, it seemed a manifestation of her will to live. Even more so when her hand moved – a sure sign of life! But that, too, was mediated through a spinal reflex.
I gave the patient some anaesthetic gas. I also gave her some opioids. Why the latter? After all, a dead patient doesn’t feel pain. In part because opioids help to lower heart rate and blood pressure directly, but also, I must admit, because I thought my patient might still be a ‘little alive’, whatever that means, and therefore in pain. Irrational on my part, yes, but the secret of life, including the definition of life, still remains the deepest and most mysterious one. Here Nature permits no eavesdroppers; never will she permit anyone to know the exact point where brain death becomes real death. At this, she draws a veil. I wanted to hedge my bets.
The woman’s blood pressure soon dropped too low. I poured fluid into her intravenous line. In the meantime, the surgeon moved hurriedly to extract her heart, clamping the large blood vessels leading both to and from it. Our fast pace betrayed another incongruence. Speed is thought to be a bit unrefined in an operating room. True, it is needed to save money, but ideally the operating room is an ordered world with calm transitions, a world without haste, except during an emergency to save a patient’s life. The visibly hasty fashion in which I and the surgeon worked made it seem like one of those urgent situations. In fact, I was trying to keep her circulation going long enough for the surgeon to tear her heart out.
I transfused a unit of blood, as excessive blood clotting, common after brain death, had made her dangerously anaemic. I turned on the warming mattress lying underneath her to keep her body temperature from dropping below 36 degrees Celsius. Brain death interferes with the body’s ability to regulate temperature, and the resulting hypothermia poses a risk to the organs. Finally, I gave her insulin to control her blood sugar level, as brain death often causes blood sugar to rise. All of these are routine lifesaving measures. In the past, I had used them to fight off death in my sickest patients, but here I had to remind myself that my patient was already dead.
The surgeon removed her heart. The irrevocable instant had come. It was as when a train starts with a violent jerk, as if to overcome a disinclination to change its state of inertia. For many in the operating room, this was the moment when the woman’s life really ended.
A minute before, I had heard the melodies of the electrocardiogram (EKG) and pulse oximeter without really thinking about them. An anaesthesiologist’s ear is so capable of adapting itself that a continuous din, like the noise of a street or the rushing sound of a river, adjusts itself completely to their consciousness. But the unexpected halt in the sounds startled me into listening – and looking. I stared over the ether screen into the woman’s now-vacant chest cavity. It was shameful and terrible to gaze upon. Part of me felt as if I had abetted a murder around the corner.
I tried to make this last sigh worthy of the moment, a sigh that only another human being could replicate
The surgeon injected the heart with cold preservative and put it in a box. His next target was the lungs. He asked me to manually give the woman one last deep breath so that he could confirm that all parts of her lungs had been expanded before their removal. The breath I gave her was slow and gentle, like a sigh. Indeed, medically speaking, it was a sigh. On ventilators, there is a function labelled ‘sigh’ which, when pressed, gives a patient a single sustained deep breath to open up the lung’s small air sacs. Almost proudly, I imagined the sigh I gave this woman to be more human than what a machine could give. Compressing the anaesthesia bag with my hand, I imagined how she might have sighed in the past, on her own, in the face of some bitter reality, some trick or force of fate, crushing her heart but also uplifting her. I tried to make this last sigh worthy of the moment, a sigh that only another human being could replicate, a deep breath that begins with disappointment, passes into resignation, and ends in acceptance. I crafted that last sigh as if it were the epilogue to a tragedy.
When the woman exhaled her last bit of sigh, I removed her breathing tube. The surgeon took out her lungs and stapled her windpipe shut. At this point, there was little for me to do, and my inactivity plunged me into a sense of nothingness. I felt I was going to gag on my thoughts if I didn’t do something. I walked away from my patient to look inside a cupboard. I opened a few drawers. Then I felt badly for doing so. Although one of us was dead, still there seemed to be two of us here. It’s as if the woman and I were friends and I didn’t want to leave my friend. I went back and stood by her head.
The surgical team removed the rest of her organs and the case finished. Here the woman and I reached a parting of the ways. I stared at her face seriously and fixedly as though I wanted to look my fill and imprint forever on my memory her image. I cannot recall for how long I looked. Great moments are always outside of time.
Our relationship proved significant. Nothing is more characteristic of the total lack of spiritual connection between myself and other patients than the fact that I have forgotten most of their names and faces. But this woman’s name and face I remember. And when I speak of memory, I do not mean something akin to a register kept in a well-ordered office, a place in which documents are laid away in store. I mean something submerged in the rushing stream of my blood, memory as a living organ in which every feeling experienced that day retains its natural essence, its original intensity, its primary historical form.

Charrier and his colleague Ludovic Dupautet en route to hospital with the organ-transport ice chest
My patient lived longer than what her death certificate says. She lived in my mind during the organ retrieval and continues to live in my memory because I do not want to forget her, and because I cannot forget her. Although I know only her general outlines, our connection satisfies some deep law of harmony underlying all life, in which every person must enter into communion with another person in order fully to live. By that standard, my patient lived past her official time of death.
When AI replaces the anaesthesiologist during organ retrievals, you, the organ donor, will not live any longer than what’s listed on your death certificate. The air inside the operating room is already cold, dry and unpleasant. Various monitors will sit on the top shelf of the anaesthesia machine, regulated by AI. Their special melodic rings will no longer be necessary, as their data will be sent along to AI in silence. Care will be delivered without the mediation of human minds, senses or hands.
Before your lungs are removed, the machine’s ventilator bellows will go up, down, up, down. Capable only of whooshing and not ringing, the bellows will seem to call sadly through the cold air to the monitors sitting above, waiting fruitlessly for a response. What a simple, insignificant movement: up, down, up, down, never getting away from the same place. It will be the only activity surrounding your head amid the metal machines, with their cold, menacing gleam. Nobody will be sitting next to you to wonder about what you were like, or about the things that distinguished your personality and made it special. A vision of the future arises: similarly deserted operating rooms with AI machines all moving automatically, while the people who used to work in them have gone off somewhere to sit dreamily on the grass beneath the sky.
Medicine has tapped a new source of organs in the form of donation after circulatory death
It seems a decidedly unpleasant environment in which to meet one’s end, and enough to discourage those on the fence from becoming potential organ donors. Rather than live a bit longer in the mind of another person, rather than have that person think about you and wonder about you, entertain irrational imaginary concerns about you, slip a little extra narcotic into your intravenous line ‘just in case’, engage in metaphysical speculations about your breathing pattern, and imagine you a friend, you will be alone on the table, and your surgery will more closely resemble a bandit raid. The machines will be determined to take everything, every organ. Reduced to financial terms, it will be as if you were left penniless.
Worse, a new danger will come to overlie the chilling sense of emptiness, scaring even more people away from becoming organ donors. Because there are already too few brain-dead donors – each year, more than 8,000 people in the US die while on the waiting list for organs – medicine has tapped a new source of organs in the form of donation after circulatory death (DCD). These organ donors are not brain dead, although many of them are unconscious. Instead, they lack circulatory or respiratory activity after being disconnected from artificial life-support systems. Without such activity after a few minutes of so-called ‘no touch’, they are declared dead, and their organs become available for donation. Their numbers have been growing over the past two decades. Today, they account for about 10 per cent of transplanted organs in the US.
The problem is that certain medicines necessarily given to these donors before death, but in expectation of death, may hasten their death. The medicines are given for the sole purpose of making their organs more viable for transplantation. Heparin, for example, prevents blood clotting, while phentolamine dilates blood vessels and improves blood flow to the organs. Yet heparin also increases the chances of bleeding into the brain, while phentolamine may lower blood pressure to the degree that a person goes into shock. Although these patients are near death for other reasons, the medicines may become their actual cause of death. This makes doctors uneasy; hence the rule not to give these medicines to donors prone to bleeding or with low blood pressure.
Yet the rule risks driving away potential donors, who will naturally think: ‘Doctors won’t give you these medicines to kill you; on the other hand, they won’t give you these medicines to help you. At some point, doctors aren’t really on your side. But when?’ As the number of brain-dead donors drops, medicine will increasingly rely on DCD donors to compensate. Already sensitised by the image of surrendering their organs to machines in a metallic desert, potential donors will fear being herded into the ‘imminent death’ category to meet some organ quota, a fear only heightened when word gets out that doctors are not always their advocates.
Currently, doctors in the US must get consent before declaring people DCD donors, but another model, called the ‘presumed consent model’, already operates in other countries and allows the recovery of organs without prior authorisation. A cascade of events threatens to turn organ retrieval into a kind of science-fiction nightmare, where organ shortages lead to medicines being given to people to preserve their organs while possibly hastening their death, all without telling them the plan or asking for their permission.
My experience in the operating room serves as a warning to those eager to cut corners and replace doctors with AI machines
Whenever people start to think about becoming an organ donor, they immediately make a leap to their own precious person. Who am I, what am I, what am I without my organs, and so forth. It is part and parcel of being a human being. That some people are willing to surrender their organs after death suggests that, to feel oneself human, they need more than merely having a whole body; they also need an atmosphere of simple humanity. To feel human, people need to feel that they occupy space in the thoughts and feelings of others. It is why they consider becoming organ donors in the first place. They imagine helping others by giving up a part of themselves in the future. In exchange, they imagine the recipients thinking from time to time about what they, their donors, were like. In that way, the donors feel a connection with whomever those recipients might be, and feel somehow fulfilled.

The surgeons arriving back at the Foch hospital with the donor’s lungs
I’d like to think that caring for my brain-dead patient satisfied some small part of this need to feel human, whether on the part of my patient before she died and who perhaps lived in expectation of becoming a donor one day, or on the part of her relatives who gave their consent to the procedure after she was declared brain dead. Either way, I connected with her or with her family.
My experience in the operating room serves as a warning to those eager to cut corners and replace doctors with AI machines willy-nilly. You don’t satisfy people’s urge to feel human by making the bridge to the next world a totally inhuman one.
The lesson extends far beyond organ donation. AI promises to make healthcare quicker, more precise, and error-free. To the degree that it replaces doctors and nurses, it portends a massive shift in medicine that seems to come every 30 years, when people are so overwhelmed by the burden of their own technological creations, they need every iota of their strength to adjust. Once again, with the advent of AI, advancements promise to put healthcare on an entirely new footing and, once again, the inevitable backlash will be there. So it was in the 1960s, when new medical technologies and procedures, such as home dialysis machines and coronary artery bypass surgery, improved life, and yet, during this same period, the medical profession’s reputation plummeted, as patients complained that doctors had grown cold and impersonal. So it was in the 1990s, when the rise of managed care promised greater efficiency at less cost, and a ‘win-win’ strategy anchored in preventive medicine, led to a patient rebellion against being treated like cattle, including their inability to choose their own doctor, and rushed visits to practitioners ‘on the plan’.
Now, in the 2020s, the stage is set for outrage, yet again. AI promises to elevate healthcare; but, to the degree that it replaces doctors and nurses, it also threatens to depersonalise patients and to wash off their distinctive colours until everyone has the same drab tint. In the crucible that looms, patients are going to rebel. And it is in the arena of organ donation, where they face death by machine, that they are likely to baulk loudest, and first.