Our understanding and treatment of mental disorders is primitive. Why is that? The burden on our society is huge. A quarter of women will have an episode of depression at some stage in their lives (it’s about half that for men). Most will never reach a doctor or be diagnosed. About 40 per cent of those who do won’t respond to the first antidepressant they are prescribed, and about 60 per cent of those won’t respond to the second. About half of schizophrenics will get better or manage to live reasonable lives: the other half will relapse or never recover in the first place. Anorexia nervosa claims the lives of more patients proportionately than any other mental disorder. But mental disorders are only one category – a rather artificial one – of brain disorders.
The treatment of multiple sclerosis, Parkinson’s disease, stroke and, above all, Alzheimer’s disease remains deeply unsatisfactory. Motor neuron disease is invariably fatal. Why should this be? Why can’t we treat brain dysfunction more effectively? There’s a simple answer: we don’t understand enough about how the brain works. But this leads to more complex questions. What do we mean by ‘understanding’? What are we actually looking for? What do we need to know?
Let’s start with the heart. Not because the ancients thought it was the seat of the emotions, or because we talk about breaking it for love; but because it can illustrate what is meant by ‘understanding’ how a part of the body works.
The essential discovery was that the heart is a pump: that is, it provides the driving force to maintain the circulation of the blood. You don’t need to know how it does that to replicate its action: a heart-lung machine pumps blood, but not in the way a heart does. So it’s an analogue, not a homologue. However, you do need to know how the circulation works to understand how the heart is built.
It was the 17th-century English physician William Harvey who discovered this, making the inspired prediction that there must be tiny capillaries that link the arteries and veins. He never saw these himself: they were observed only after the discovery of the microscope. But as soon as the design of the circulation is known, it is obvious that blood entering the right side of the heart from the body (low in oxygen) must go to the lungs, be oxygenated there, and return to the left side, before being pumped out to the body again. Blood must go only one way, which explains why there are valves in the heart that prevent reflux. This also explains why damage to those valves impairs the ability of the heart to send blood either to the lungs or the body, depending on which valve is damaged. So now very successful surgical procedures can be developed that replace damaged valves, in a form that replicates their function.
The next question is how the pump works. How does the heart muscle produce a coordinated squeezing action that propels the blood? We now understand the physico-chemical processes that allow muscles to contract. We also understand that there is a system in the heart that coordinates the contraction of each of the four chambers. So if the heart begins to beat irregularly, we know what to do. And we have discovered that the heart has a blood supply of its own, and that this can get blocked, which damages the heart. So we have devised ways of unblocking the coronary vessels, and, because we know why they become blocked, we can reduce the likelihood of this happening.
There are many ways of studying heart function in the living person. Some are rather recent: the number of recognisable heart diseases has increased not because more have occurred but because we have become so much better at distinguishing the different ways a heart can malfunction. So treatment has become more effective and targeted: we know what has gone wrong and, to an extent, what to do about it. Not everything, of course; not yet. But each level of understanding has lead to particular advances.
If all else fails, we can even transplant hearts, something that was once impossible. We can do it because we understand a good deal about how the immune system works, and how the body recognises ‘self’. The heart is no longer a mystery; the principle on which it works is understood. There is still quite a lot to be learnt, of course. But the path to that knowledge is reasonably clear.
Move to the brain and our clear-sighted view turns suddenly foggy. Like the heart, the brain is made up of specialised cells, the neurons. We understand quite well how each neuron is activated, and how it passes this activation onto the next neuron. But now comes a major problem: we know how a collection of heart muscles makes a pump, but not how a collection of neurons makes a thought, a memory, a decision, an emotion. We know it must be a network of neurons: and simulations show us that such assemblies take on properties that are very difficult to predict from the way individual neurons behave. But what is it about such an assembly that represents what we know a brain can do?
Neurons work in a particular way: the brain is an electrochemical machine. Each neuron is activated by a chemical released from another neuron: this then initiates an electrical signal that passes down the neuron’s fibre and, in turn, releases another (or the same) chemical onto the next neuron. But this isn’t a simple chain: each neuron can communicate with about 10,000 others, meaning that the permutations are unbelievably huge. There are around 100 billion neurons in the human brain, and around 1,000 trillion possible connections.
Even so, suppose that we knew at each instant what each neuron was doing – what chemical it was releasing and where. Suppose further that we could relate this to something the brain was doing at that moment (say, making you hungry, or seeing someone you knew) – a circumstance way beyond contemporary neuroscience. Would we really ‘understand’ what we were observing? Would we ‘know’ why this pattern represented a thought, a perception, a motivational or emotional state? Could we then predict what a different state of mind (say, thirst, or recognising a banknote) might require? There is no theory of neural function that would allow us to do this, beyond a vague generalisation that the particular activity of a neuronal assembly or network was responsible (and even this might vary in different parts of the brain). We don’t actually know what to look for.
The mysterious, unfathomable gap between psychology and neuroscience bedevils not only psychiatry, but all attempts to understand the meaning of humanity
We understand the brain at another level. Different parts of the brain do different things. We know that there are separate areas that generate movement, receive sensation, process information from the eyes and so on (though the boundaries between them are indistinct). For example, we know that visual information is passed progressively through a series of visual detection areas, each extracting one element of the things we see (shape, colour, movement, etc). Then – the mystery. Somehow the brain fuses all this together so we see one object, with all its attributes, as a single experience. We don’t understand how this happens. Though we can measure the activity of the neurons in these various areas, we can’t construct a plausible scheme whereby this activity is responsible for the phenomena that we know occur there.
The problem of relating events at the level of neurons with the known functions of the brain is a critical one. Our knowledge of other organs is no help: we can’t extrapolate what we know about the heart, the liver, even the immune system (itself immensely complicated) to learn how to really understand the brain. Psychology is a description of what the brain does: neuroscience aims to describe how the brain works. The mysterious and seemingly unfathomable gap between them bedevils not only psychiatry, but all attempts to understand the meaning of humanity. We are what our brain is, and our wonderful hands allow us to carry out its commands. But if we can’t explain precisely how we decide to make a movement, let alone how we learn to perform it more accurately, how can we even attempt the greatest task of all: explaining how the brain produces consciousness?
Here we see the seductive power of analogues. We can build a computer that, in many (if not, so far, very advanced) ways replicates what a human brain can do. It can do calculations that are beyond most, if not all humans. It can make decisions. It can learn. It can store information. It can even fool a human into thinking that he or she is communicating with another human. Does this tell us anything about how our brains do similar things?
Not at all. An electronic computer is not an electrochemical machine. It works in quite different ways from a human brain. It is mimicking what a brain does, not replicating it, just as an electronic clock mimics a mechanical one. Artificial intelligence can assist humans, could replace them, might even eliminate them: but computer designers don’t need to know how the brain works, any more than a manufacturer of a heart-lung machine needs to know about the heart. In each case, we need to know only what it does.
If the mechanic in your garage doesn’t understand how your car’s engine is built, then he is not going to be able to say why it’s making that clunking noise either, or how to put it right. Ask any psychiatrist what happens in the brain to make people depressed, and she will probably mention serotonin. Serotonin is one of the many chemicals that neurons release. The psychiatrist singles out this one because most of the drugs used to treat depression seem to work by altering its levels in the brain. Altering noradrenaline (a related neurotransmitter) is also effective.
At a psychiatrists’ clinic, there are no machines or blood tests that aid diagnosis. How different from the cardiologist next door!
And yet, there is no evidence at all that the levels of serotonin or noradrenaline in the brains of depressed people are any different from normal. The logic is flawed: you cover a cut on your finger by a sticking plaster, which helps recovery; but the cut was not caused by a lack of sticking plasters. So altering serotonin can speed recovery in some people – and there are those who question even this – without telling us anything about what depression is or how it occurred in the first place.
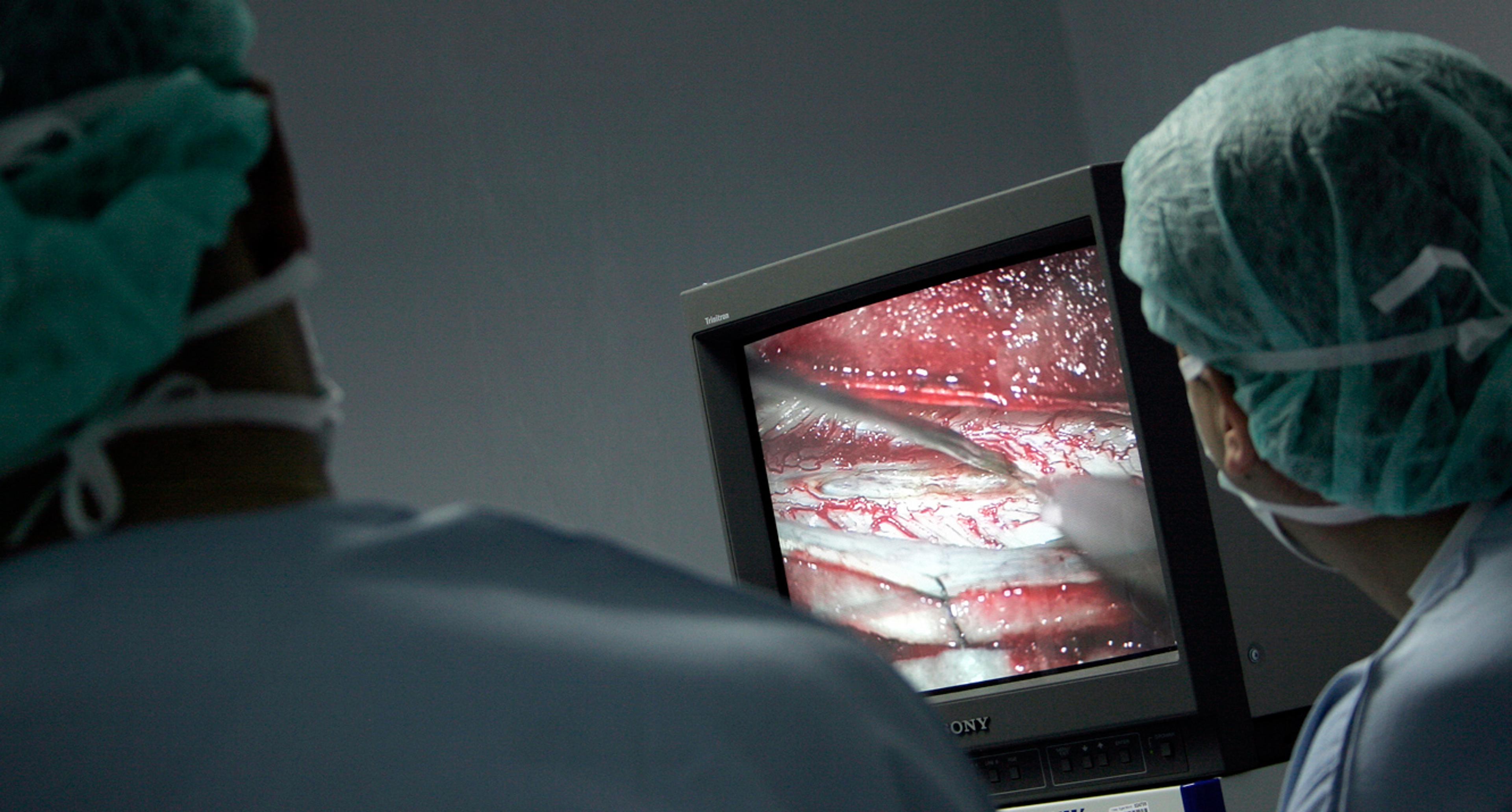
At present, a pathologist looking at the brain of a depressed person could not distinguish it from the brain of someone who was mentally well. (Given the brain of someone who’d had multiple sclerosis, he could see the scars that the disease makes.) And if you visit a psychiatrists’ clinic, you will find no machines or blood tests that aid diagnosis. How different from the cardiologist next door!
Things are a little better for neurologists. Modern imaging techniques can often reveal what has gone wrong in the brain, because these illnesses are commonly caused by observable changes in its structure. Here, the problem is knowing what to do about it, unless it’s something removable like a tumour. Actually, this is a little unfair to the state of neurological medicine. There are circumstances in which treatments can be at least partially effective, and this is an active area of research. The treatment of multiple sclerosis, for example, has improved a good deal during the past decade, and there are promising signs that we might be able to help the damaged spinal cord to repair itself before too long. But for now, neurologists have very limited treatments, and this also reflects our ignorance of how the brain works or how to fix it.
Mental illnesses, as distinct from neurological ones, are diagnosed and classified entirely on symptoms. There are no objective tests, no blood tests, no scans, no recordings. There is no other area of medicine to which this still applies (at one time, all medicine was based largely on symptoms). A wide range of techniques are available and are used both clinically and as part of research on the brain. They are very useful; indeed, essential. But not in psychiatry. Psychiatry has tried hard to make the use of symptoms both reliable and consistent, with mixed success.
The American Psychiatric Association developed a formal classification of symptoms, which has been very helpful for psychiatrists in different clinics or countries to diagnose mental illnesses in the same way. But this system has highlighted two major problems: each illness has a large and variable number of symptoms attributed to it, so this can conceal distinct disorders within each category; and the symptoms for each disorder overlap to some extent, thus blurring the distinction between diagnoses. There is a further complication: the brain differs between people, both genetically and as a result of experiences. So a given disorder in the brain might well give rise to different symptoms depending on the individual concerned. The reason for the comparatively few psychiatric diagnoses is that we don’t know how to analyse them more minutely.
until we have precise knowledge about what distinguishes the brain of a depressed person, we won’t know how to put it right
It is surprising that there are rather few psychiatric disorders. But the diagnostic system itself has become dignified as part of the professional structure of psychiatry, difficult to challenge or to change. The history of medicine shows us that classifying illnesses (the first step to understanding them) on symptoms alone is always inaccurate, and underestimates the complexity and variety of the ways in which an organ or system can become deranged. For example, shortness of breath (dyspnoea) was once a diagnosis: now we know that it can be the result of many underlying conditions, including several in the heart, lungs, blood or brain (for example, anxiety).
Let’s look at depression again. We have some ideas about which parts of the brain are responsible for generating emotion, and even some (rather sketchy) information about which parts of the brain might be dysfunctional in depression (assuming this is a single disorder, which it most certainly is not). But until we have precise knowledge about what distinguishes the brain of a depressed person (or a schizophrenic, or an obsessive one, or whatever), we won’t know how to put it right.
This doesn’t necessarily mean that we need to understand how this part of the brain generates the experience we call ‘depression’, any more than we must understand how the brain generates consciousness to develop effective anaesthetics. As we’ve seen, partial knowledge is sometimes enough to offer effective remedies. Edward Jenner didn’t need to know anything about the immune system to develop vaccination in the late 18th century: he simply observed the incidence of smallpox in those looking after cows. He had no idea how vaccination works; but that doesn’t prevent it from being highly effective. It’s feasible that we could, by chance or good luck, discover a highly effective remedy for depression without understanding why or how it works: the history of medicine is full of such serendipity (for example, the discovery of penicillin). But for a full understanding, we need to know what goes wrong.
Why don’t we already understand more about the depressed brain?
Let’s shift focus again, this time onto cancer. Treatment of cancer has advanced spectacularly over the past 100 years – though, as we all know, there is much more to be done. Nowadays, about three-quarters of children with acute leukaemia will survive. The story is not so encouraging for some other cancers, but the trend is obvious, and there is considerable excitement about the arrival of new treatments.
It is not so for psychiatry: most of the drugs have either been around for many years, or are modifications of old ones (I am not assuming that all effective treatments for mental illnesses are, or will be, drug-based). The reason for the bright prospect for cancer is that there are credible and validated models for research. Animals develop cancer, or can be made to do so. These cancers are very similar to human ones. Cancerous cells can be grown in dishes, where they behave in recognisably cancerous ways. We understand that cancer is a genetic disease: it’s caused by mutations in genes that control a cell’s growth. We know many of the genes, and how they change.
This fact, together with our possession of good experimental models, is leading to a new generation of treatments. For example, drugs based on antibodies that target and kill cancer cells have been developed, and more are in the pipeline. They promise much better treatments than the current, rather crude, chemotherapy, with its limited effectiveness and serious side-effects. So there are lots of reasons for hope with regard to cancer.
The tunnel towards psychiatry, however, remains quite dark. Despite plenty of claims to the contrary, neuroscience has no credible experimental model of any psychiatric illness. Neither can we grow neurons in a dish in a way that represents a psychiatric disorder. So we can’t study it very well. Many large pharmaceutical companies have simply given up research on new drugs for mental illness: they can’t see the way to go; the hope for the future lies more with small biotech start-ups. It’s up to academic neuroscience to provide many of the answers, but the obstacles, technical and theoretical, as you can see from the above, remain daunting.
Alzheimer’s disease has moved from psychiatry to neurology because we know something about the pathological changes in the brain that underlie it
There are more neuroscientists alive now than ever, and governments and other organisations announce concerted programmes to solve these problems. Some are not very well‑thought‑out. But at least the overall problem is being recognised. The current scientific climate is very focused on the biology of the cell, or the genes that cells contain or activate. We know more about the cells that make up the brain, and about how they connect or modify their connections. The recent advances in our understanding of the genome have had effects on brain research just as on every other field. These are exciting times for molecular and cell biology, and for genetics. Yet the jump to the function of the brain as an organ still seems insurmountable. Which is why psychiatry will go on being the way it is now for some time.
But one day, someone, somewhere will make the critical step, or steps, and we will enter a new world of psychiatry. One that can relate what psychiatrists see in their patients to what can be seen in the brain. It might be understood at a cellular level: which neurons are malfunctioning? Or at a chemical one: are there abnormal chemicals being produced? Or at a ‘systems’ level: are there abnormal networks or assemblies of neurons operating? For a true understanding, we would need to be able to extrapolate from each level to the others in a logical and meaningful way. The critical test, as in other areas of science, is whether this will enable us to predict a neurological or psychological state just from looking at this data. And then we need to know how to put it right. Perhaps at this point we will see reconciliation of the longstanding divorce of psychiatry from neurology.
It’s interesting that Alzheimer’s disease has moved from the province of psychiatry to neurology. Why has it been reclassified? Because we now know something about the pathological changes in the brain that underlie it. Medical scientists can see what’s going wrong in an Alzheimer’s brain. The disorder itself has not changed, but our understanding of it has. It seems reasonable to hope that this will eventually lead to effective prevention – something all but impossible to imagine without detailed knowledge of the neurological problem. Let’s look forward to the day when all the rest of psychiatry goes the same way.
Then the scourge of mental illness, a tragic and crippling burden for individuals and society, might at last begin to be lifted.