In 2000, Jeane Newmaker took her adopted 10-year-old daughter Candace to an ‘attachment therapy’ retreat designed to increase their emotional bond. While there, Candace underwent an intervention that’s supposed to replicate the birthing process. Therapists wrapped her in a flannel sheet and covered her with pillows to simulate a womb or birth canal. Then they instructed her to fight her way out while four adults (weighing nearly 700 lbs in total) tried to stop her. Candace complained and screamed for help and air, unable to escape from the sheet. After 70 minutes of struggling, pleading that she was dying, and vomiting and excreting inside the sheet, Candace died of suffocation. This tragic case highlights an important but often overlooked aspect of psychological interventions designed to help people – sometimes they can be harmful, or even fatal.
Candace Newmaker’s death is a shocking and obviously recognisable example of an alleged treatment causing immense harm. However, there are innumerable psychological treatments on offer, many of which are not so obviously harmful but that can also carry risks. Consider that, before her rebirthing treatment, Candace underwent other forms of attachment therapy, such as ‘holding therapy’ wherein her mother Jeane held her for an extended, uncomfortable period and restricted her movements. Candace was also pinned under her mother during a session of so-called ‘compression therapy’. Throughout these different psychological treatments, her mother licked her to induce rage. These strange interventions are perhaps harmful too, but less strikingly so than the rebirthing procedure. Yet they all continue to be practised in some US states and elsewhere around the world.
Assessing whether a psychological treatment causes harm can be surprisingly difficult, and intuition is an unreliable guide. Take the popular school programme Drug Abuse Resistance Education (DARE) founded in Los Angeles in 1983. The idea of DARE, consistent with the wider ‘war on drugs’ in the United States, is straightforward: uniformed police officers visit classrooms to warn children and teens about the dangers of drug and alcohol use, thereby reducing underage use of alcohol and illicit substances, or so it is hoped. On the surface, DARE appears to be potentially beneficial and unlikely to harm. However, in 2001, the US surgeon general deemed DARE ineffective. Decades after it was developed, and despite millions of dollars spent annually on its implementation, the data indicated that DARE was no better than doing nothing.
Or was it worse than that? Was DARE potentially leading to an increase in alcohol and drug use among children and teens? The history of interventions such as rebirthing and DARE highlights important questions that should concern anyone involved in therapy, clients and therapists alike: how do we know if a certain treatment or intervention helps people as proclaimed, or if it is ineffective, even potentially harmful? And whom do we trust to make these judgments?
In the US, one might assume a government agency is responsible for the oversight of psychological interventions such as mental health treatments or larger intervention programmes. After all, the Food and Drug Administration (FDA) regulates numerous products including food, tobacco, some supplements, pharmaceutical drugs, vaccines, medical devices and cosmetics. Yet the FDA has no oversight over psychological interventions, and neither does any other agency. And while every state and territory in the US has licensing boards to oversee mental health practice and safeguard the wellbeing of the public, these boards rarely prohibit types of treatment or interventions; instead, they focus on unethical therapist behaviour, such as sexual relationships with clients and the false claiming of qualifications.
Nor are clients protected from given forms of therapy or large-scale interventions by state or federal law. A notable exception is that about half of US states have banned ‘conversion therapy’ or ‘reparative therapy’ for minors, which attempts to change their sexual orientation. But we know of no other psychological interventions that are so widely banned by law. Importantly, Candace Newmaker is not the only victim of attachment therapies such as rebirthing and, since her death, only two states have outlawed the practice. Without a governing body or lawful regulations, the people providing psychological interventions and the people receiving those interventions are left to figure out on their own whether there is any potential for harm.
Negative experiences from mainstream mental health care are seen among many ethnoracial minority clients
Unfortunately, history is replete with popular mental health interventions that turned out to be harmful, or even deadly. In hindsight, it may seem all too easy to disregard trepanning (ie, curing ‘madness’ by drilling holes in the skull to release evil spirits), leeches and electric eels as ridiculous ‘treatments’, but harmful treatments – however abhorrent or ridiculous they seem now – have a way of sticking around. For instance, lobotomies were used in the late 20th century for decades after their barbaric nature was recognised; similarly bloodlettings, which likely contributed to the death of George Washington, continue to be used in some parts of the world today. But harmful therapies are not limited to these centuries-old treatments.
Although viscerally harmful treatments such as rebirthing are mercifully rare nowadays, less dramatic but still significant harms arising from psychological practices are more widespread. You might imagine that more conventional forms of modern therapy as delivered by a psychologist, counsellor or clinical social worker cannot be harmful because the treatments involve ‘just talking’. Regrettably, this is not the case. For instance, a survey published in 2018 of more than 14,000 clients who’d undergone therapy with a qualified professional in the NHS in England and Wales found that 5 per cent reported experiencing unspecified lasting harmful effects from the experience; similar effects were reported by 14 per cent of clients in a survey published in 2021 (other studies suggest these ill effects are likely to include worsening symptoms and relationship problems). An extensive literature also documents negative experiences from mainstream mental health care among many ethnoracial minority clients (eg, overdiagnosis of severe mental illness among Black Americans) that likely reflects both prejudices and cultural insensitivities.
It is important to state that, globally, most psychotherapies are helpful and not harmful. Meta-analyses (which, in short, combine data across numerous clinical trials to calculate the ‘average’ treatment effect) have consistently shown that receiving any bona fide psychotherapy (that is, a therapy with a clear rationale that is grounded in psychological science) more often leads to beneficial effects compared with not receiving any therapy. For instance, a meta-analysis published in 2021 showed that receiving any bona fide therapy compared with no treatment more than halves the chances of psychological deterioration in children. However, these are averaged effects, and the devil is in the details – for many psychological interventions, the cost-benefit ratio is less clear.
To better understand how upwards of one in 20 clients could be harmed from psychotherapy, or whether programmes like DARE are harmful, it’s important first to determine what we mean by harm, and to distinguish among the different forms that harm can take in these contexts.
One not so obvious form of harm is an ‘opportunity cost’ – even if somebody undergoes a treatment that does not make their symptoms worse, but is merely ineffective, then in a sense they have been harmed because they’ve missed out on a treatment that could have helped. Some opportunity costs will be difficult if not impossible to avoid because it’s so hard to predict who will benefit from different forms of therapy. However, some therapies have opportunity costs that are eminently knowable. DARE, as assessed by the US surgeon general, would fall into this category: it absorbed exorbitant amounts of taxpayer money and student time that could have been used for an effective substance-use intervention instead.
Teaching people to punch when angered leads to more anger and punching
A more obvious form of harm is when a treatment causes short-term deterioration in clients, with no prospect of any long-term benefit, and sometimes the chance of longer-term harm. A clear example is ‘cathartic interventions’ that promise relief by directing people to express difficult emotions in a purge-like manner, such as punching pillows when angry and yelling as loudly as possible when distressed. Such practices date to the times of Sigmund Freud in the late 1800s and ‘primal scream therapy’ in the 1970s, and lend themselves to the rising popularity of ‘smash rooms’ in which people pay to ‘therapeutically’ destroy items such as televisions and toasters with a hammer. Despite their popular appeal, copious research indicates that, as a means of dealing with difficult emotions, these approaches have the opposite of the intended therapeutic effect, actually increasing anger and distress. Simply put, teaching people to punch when angered leads to more anger and punching. Furthermore, most often the therapists providing these treatments are unaware of their harmful effects. This is also likely the case for therapists who recommend mindfulness interventions to their clients without reservation, failing to consider that, in a minority of users, mindfulness can cause adverse events such as anxiety, depression and unpleasant dissociation.
Similarly, some therapists, including celebrated pioneers, have been seemingly ignorant of the harms caused by conversion therapy, such as depression, low self-esteem and impaired sexual function. For example, Albert Ellis reported using rational emotive behaviour therapy (REBT) – a forerunner to modern cognitive behavioural therapy (CBT) – to change a man’s sexual orientation:
In this case of a 35-year-old male who entered therapy because he was severely troubled by a fixed pattern of homosexuality, a swift frontal attack was made by the therapist on the basic assumptions or philosophies illogically underlying the client’s symptoms. In the course of this attack, the client was shown, by the therapist’s rigorously unmasking and then inducing the client himself to contradict and act against his irrational beliefs, that his homosexual pattern of behaviour and his other neurotic symptoms were not hopelessly ingrained, and that he himself could control his own destiny by changing his assumptions … As he began to change the fundamental irrational beliefs that motivated his homosexual and neurotic behaviour, the client’s symptoms almost automatically began to disappear and he was able to change from a fixed, exclusive homosexual to a virtually 100 per cent heterosexually oriented individual.
‘Virtually’ indeed. Similarly, in A New Guide to Rational Living (1975), the revised edition of his bestseller, Ellis wrote:
Jack M, a compulsive or obligatory homosexual, came to therapy at the age of 25 … After 10 years of highly promiscuous homosexual behaviour, including one arrest and a recent attempt to blackmail him at the school for boys at which he taught, Jack decided he’d better attempt to ‘go straight’. And he came to see me (AE) with the knowledge that I, unlike a good many therapists, strongly felt that compulsive homosexuals definitely could change … His sexual interest in males considerably diminished and he felt sure that whatever interest he had, he could control, or occasionally act out uncompulsively.
Ellis’s REBT has helped untold numbers of clients, but his promulgation of conversion therapy was wrong then and wrong today. Perhaps Ellis realised this: the far-fetched story of Jack M was removed from later editions of his influential book.
So, psychological harm can take many different forms, and it’s not always obvious, even to the most talented therapists. Thankfully, clinical researchers have highlighted the problems with purging emotions in a cathartic manner, and they continue to study other forms of potentially harmful interventions. An influential figure in this field until his untimely death in 2020, the US psychologist Scott Lilienfeld reviewed this research and outlined numerous potentially harmful psychological and behavioural interventions, which included attachment therapies such as rebirthing. Unfortunately, since the publication of Lilienfeld’s landmark paper in 2007, seemingly little has changed in clinical practice; most of the interventions he outlined are still employed today.
Harmful treatments persist, ironically, in part because the same research processes that can identify safe and effective interventions can also mask the harmful ones. DARE, for example, has been tested repeatedly in forms of randomised controlled trials, the gold standard for health intervention research. These trials have often provided a range of outcomes that could be taken to indicate either that the intervention helps, is ineffective, or is harmful. When the scientific literature on an intervention grows sufficiently large, it becomes all too easy for biased individuals to focus on studies that confirm what they want to see, and all too difficult for more objective investigators to separate high-quality trials from the more cringeworthy studies.
Our own research team (the present authors, along with the PhD students Robyn Kilshaw at the University of Utah and Ryan Wong at University of Victoria in Canada) has tried to address this problem for some potentially harmful treatments. Using methods we wrote about for Aeon previously, we studied the credibility of all the available research evidence for the psychological interventions Lilienfeld reviewed in his 2007 paper, leading us to analyse 70-plus randomised controlled trials. As we recently reported in the journal Clinical Psychology: Science and Practice, the results for each treatment were often ambiguous – unfortunately, we found more cringe than quality. For example, the statistical analyses for many trials were often reported so sparsely that we could not independently verify their accuracy. Across the board, the clinical trials for all the treatments we examined also exhibited signs of having insufficient numbers of participants, making it impossible to draw reliable conclusions about their effectiveness. Worryingly, we also found that the claimed statistical support for treatments in the clinical trials was consistently and implausibly positive, given the trials’ modest sample sizes.
It’s unethical to continue practising CISD without some new compelling evidence that it helps first responders
These methodological patterns are beyond concerning; many of these treatments (eg, boot camps for conduct disorders; expressive-experiential psychotherapies) have existed for decades, yet uniformly lack evidence from which one can solidly conclude whether they work. However, despite the limitations of this literature, we were able to extract some signal from the noise for four treatments. The news was not all bad: there was robust evidence that grief therapy – a treatment for individuals following loss of a loved one – can help those who receive it, and we found no evidence that it harmed them. Unfortunately, the same could not be said about the other three interventions for which sufficiently robust evidence allowed for firmer conclusions:
Critical incident stress debriefing (CISD)/psychological debriefing
CISD and similar interventions are a popular option for first responders such as police officers and firefighters. The treatment is meant to forestall potential mental health problems, particularly post-traumatic stress disorder (PTSD), by intervening in the immediate aftermath of a severely stressful event. Our statistical analysis found that, in a best-case scenario, CISD provides no benefit, while in the worst-case it increases PTSD symptoms. Because most people do not develop PTSD following a traumatic event, it might be that harm arises from compelling people to discuss and re-experience the traumatic moments in a setting in which they are uncomfortable, which interferes with the natural healing process. We consider it unethical to continue practising CISD without some new compelling evidence that it helps first responders. (For example, we would be interested in the results of a large, preregistered randomised control trial of a modified form of CISD that is more congruent with existing psychological research on healing from trauma.)
Scared Straight
Scared Straight is a psychoeducational programme that was first popularised by a 1978 documentary of the same name, and then reintroduced to modern audiences via the TV series Beyond Scared Straight (2011-15), which ran on the A&E cable network in the US. Scared Straight and similar interventions expose adolescents who have been found guilty of committing a crime to a real prison and real-life prisoners. The intention is that the prisoners will scare the adolescents onto the ‘straight and narrow’, including using threats of physical and sexual assault. Our statistical analysis suggested that, in a best-case scenario, Scared Straight has a tiny harmful effect. You read that right – the most optimistic interpretation of the data is that Scared Straight interventions hurt teenagers. Conversely, in a worst-case scenario, Scared Straight meaningfully increases the odds that adolescents who complete the programme will reoffend (perhaps via increased socialising with the other teenagers on the programme; reinforcement of antisocial behaviour via ‘tough love’, or a myriad other possibilities). Again, as with CISD, our analysis indicates that Scared Straight-type programmes should cease.
DARE
What about DARE? We found that, in a best-case scenario, DARE has a negligible beneficial effect; in a worst-case scenario, it has a similarly tiny or negligible harmful effect. In other words, our statistical results indicate that DARE is a poster child for opportunity costs: children who participate in DARE are unlikely to be helped or harmed by it (maybe because ‘information-only’ interventions do little to inspire motivation and behaviour change), and so the time and money spent on DARE could be better spent on anything that is actually of benefit.
Our analyses were limited by the substantial problems in the clinical trials that we’ve noted. Additionally, they were constrained by the lack of availability of clinical trials for any given treatment. For instance, we could not assess some of the interventions Lilienfeld chronicled, including the attachment treatments that killed Candace Newmaker, because no one has yet had the gall (thankfully) to test such interventions in rigorous clinical trials. However, for those treatments, the documented cases of lethal harm should be convincing enough to consider their use as unequivocally unethical. But many other interventions are still poorly researched, and it is an open question whether and for whom they are helpful versus harmful.
It is concerning that all the potentially harmful treatments we’ve discussed, and many more, still maintain a foothold in mental health treatment and are easily available throughout the US and in many other countries. If you are an adult US citizen, in almost any state you can find a licensed provider who will try to change your sexual orientation (laws ban the practice only for minors). If you are still interested in undergoing a questionable attachment therapy, then finding a practitioner is also just a Google search away. Moreover, many of these treatments are touted on podcasts, television shows and films. Unfortunately, the average person seeking a psychological intervention, often desperate for help, cannot be expected to possess knowledge of health statistics and methodologies to understand the potential for benefit or harm. Additionally, many people likely assume that interventions often seen in the popular media – such as Scared Straight, which has spawned five TV movies and a multi-season TV series spanning four decades – are accepted and effective.
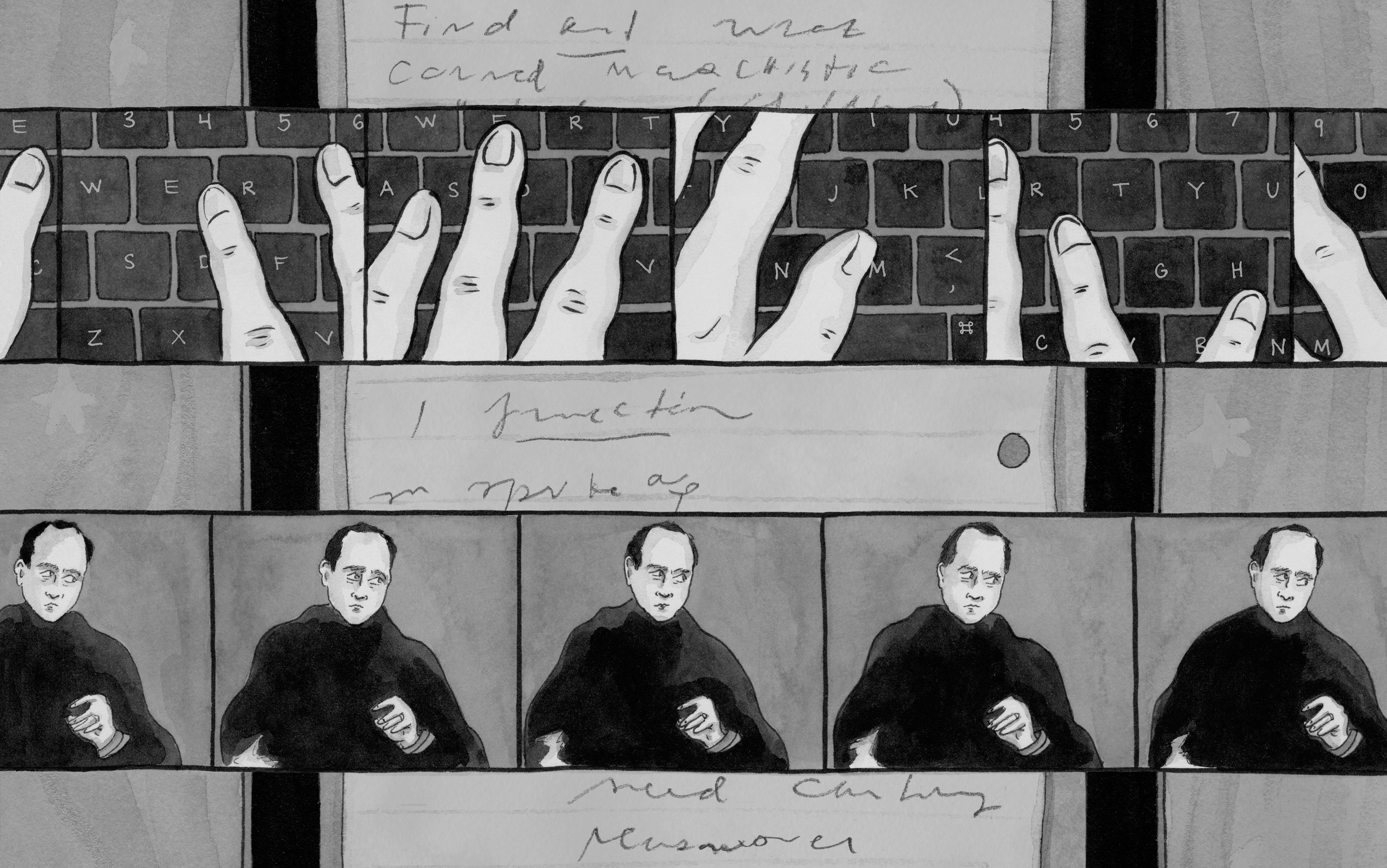
It often falls upon mental health providers to safeguard against harm, but psychologists, social workers and other kinds of mental health therapists are also subject to human biases, such as confirmation bias – the tendency to seek out evidence to justify one’s existing beliefs. Like all of us, therapists are also often much more swayed by their personal, anecdotal experiences than the scientific literature. The individuals who killed Candace Newmaker and most clinicians who continue to practise ineffective or potentially harmful interventions are not devious individuals looking to harm the public. Rather, these individuals simply, but regretfully, rely on their own perceptions above what has been shown, at scale, scientifically.
The reality is that many healthcare providers lack the scientific training necessary to understand the statistical and methodological nuances of clinical trials. For the typical therapist, many layers of human bias obfuscate the outcomes of the treatments they provide. Most will see their treatments as helpful, even when they are not. Simply put, oftentimes the evidence therapists use to judge the efficacy of their interventions (eg, the client says they are doing better, the client ‘looks better’) are the least reliable indicators for that purpose. Indeed, many apparent gains might not be real, or could be attributable to other factors having nothing to do with the therapy, such as a placebo effect, or a reversion to a more typical state of mental health.
Replacing Scared Straight and CISD with literally no intervention whatsoever would be more beneficial
We urge therapists to remember that good intentions are not sufficient for fulfilling their ethical duty to do good (beneficence) and to do no harm (nonmaleficence). We also remind them – as we, the authors of this essay who are clinicians, remind ourselves in our own practices – how commonly confirmation bias can cause one to make overly optimistic armchair assessments of client improvement. If and when evidence emerges that a treatment they use has the potential to harm, clinicians should reconsider their use of that treatment despite any allegiance they might have to it. We, the authors of this essay who are clinicians, have also taken this lesson to heart, discontinuing our use of potentially harmful therapeutic techniques we were trained in and felt attachment to. Additionally, if evidence of a treatment’s benefit is lacking, yet credible evidence of possible harm exists, these interventions should be subjected to what we call ‘psychological reversal’: for safety, they should be retired. Where possible, these treatments could be replaced with interventions that have actual evidence of benefit, though we want to stress that the evidence from our review suggest that replacing interventions such as Scared Straight and CISD with literally no intervention whatsoever would be more beneficial.
While it is clinicians’ responsibility to not provide harmful interventions, individuals seeking treatment can take steps to protect themselves too. The study we mentioned – that showed 5 per cent of clients reported lasting harmful effects from therapy – also found that it was those clients who were unsure about what type of therapy they’d received who were more likely to say they’d experienced harm. Conversely, those who’d sought more information about a treatment were at less risk. This suggests that putting full faith in a therapist could be problematic. To any readers of this essay undergoing therapy, we want to reassure you again that most clients are still helped by therapy, but we do recommend that you request that your therapist is up to date on treatment research, and also that they are able to present you with evidence that the treatments or interventions they are providing have been rigorously tested. We especially encourage you to challenge your therapist in this way if something about the treatment is atypical, such as if it involves physical contact. Your therapist should have evidence their treatments work and share with you any concerns about potential harms. If your therapist never requires you to complete some sort of assessment of your progress – even a symptom checklist – then we suggest you see this as a red flag.
Fortunately, there is much room for growth in improving safeguards against harmful therapies. Policymakers, funders and government agencies need to be aware that some of the interventions they are fiscally supporting may be ineffective or potentially harmful. They should review the concerns in the scientific literature about an intervention, and consult with clinical scientists and practitioners (including those who are not users of the treatment) before providing it with additional support and resources. At some point, monetary backers have to deploy the stage hook: if evidence consistently shows that a well-intentioned intervention they financially supported either has no effect on clients or actively harms them, they need to exit their funding, stage right. And if the intervention persists? The public may need to give regulatory agencies more powers to ban harmful psychological interventions, to be able to tell those individuals or organisations using such approaches: ‘Don’t you DARE.’